Emphasizing Payer-Provider Synergy
Our AI solution excels in proactive fraud prevention, combing real-time analysis with the ability to adapt to new challenges, ensuring unparalleled protection and system integrity in healthcare
1
Fraud Detection
Advanced AI tools to detect and prevent fraudulent activities
2
Compliance
Automated checks for compliance and error detection in real time
3
Quality of Care
AI insights to improve member experience and care delivery
It's like having a lawyer & contract expert trained on your materials!
Foundational AI
In today's rapidly evolving digital landscape, AI technology isn't just an advantage-it's a necessity.
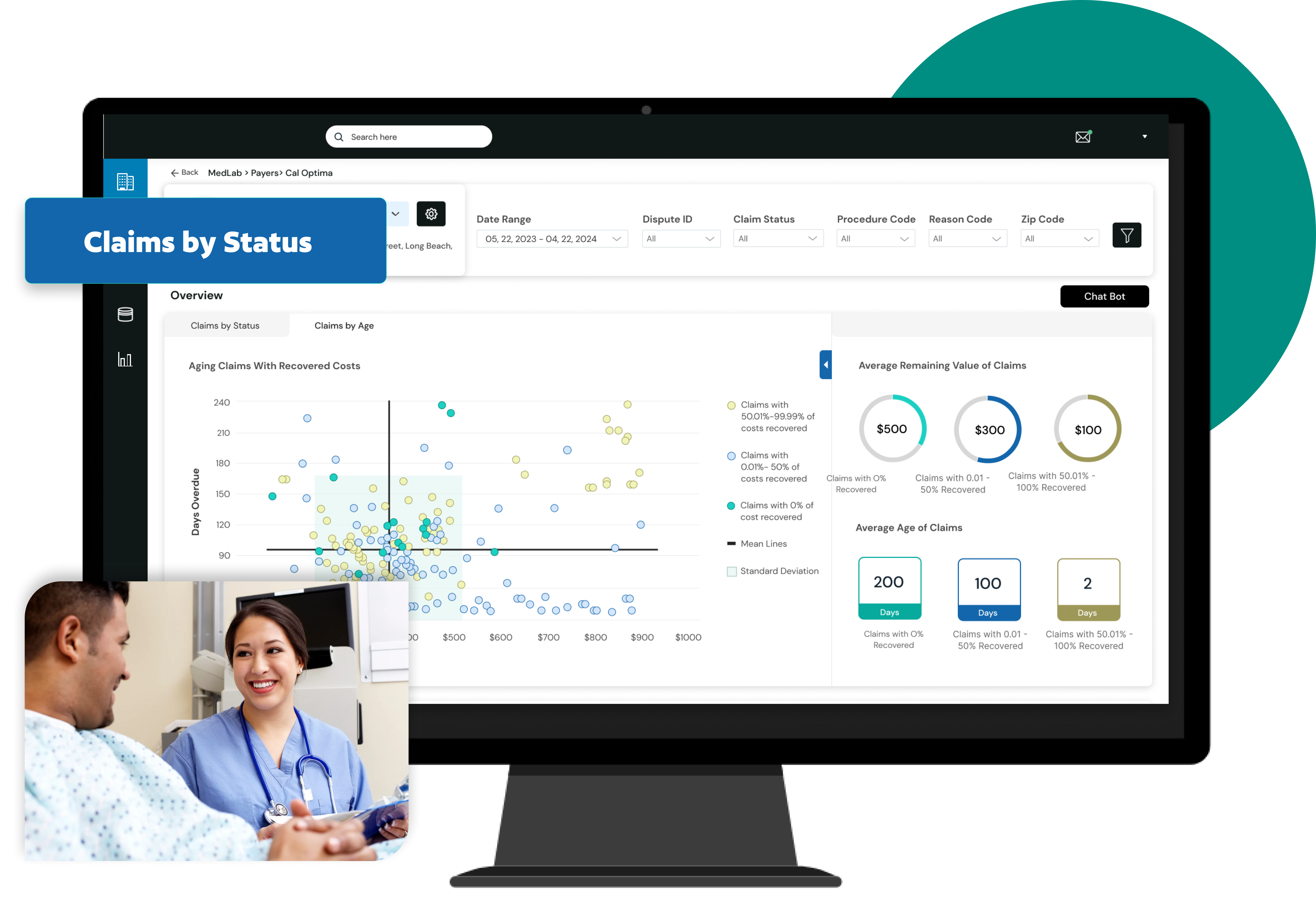
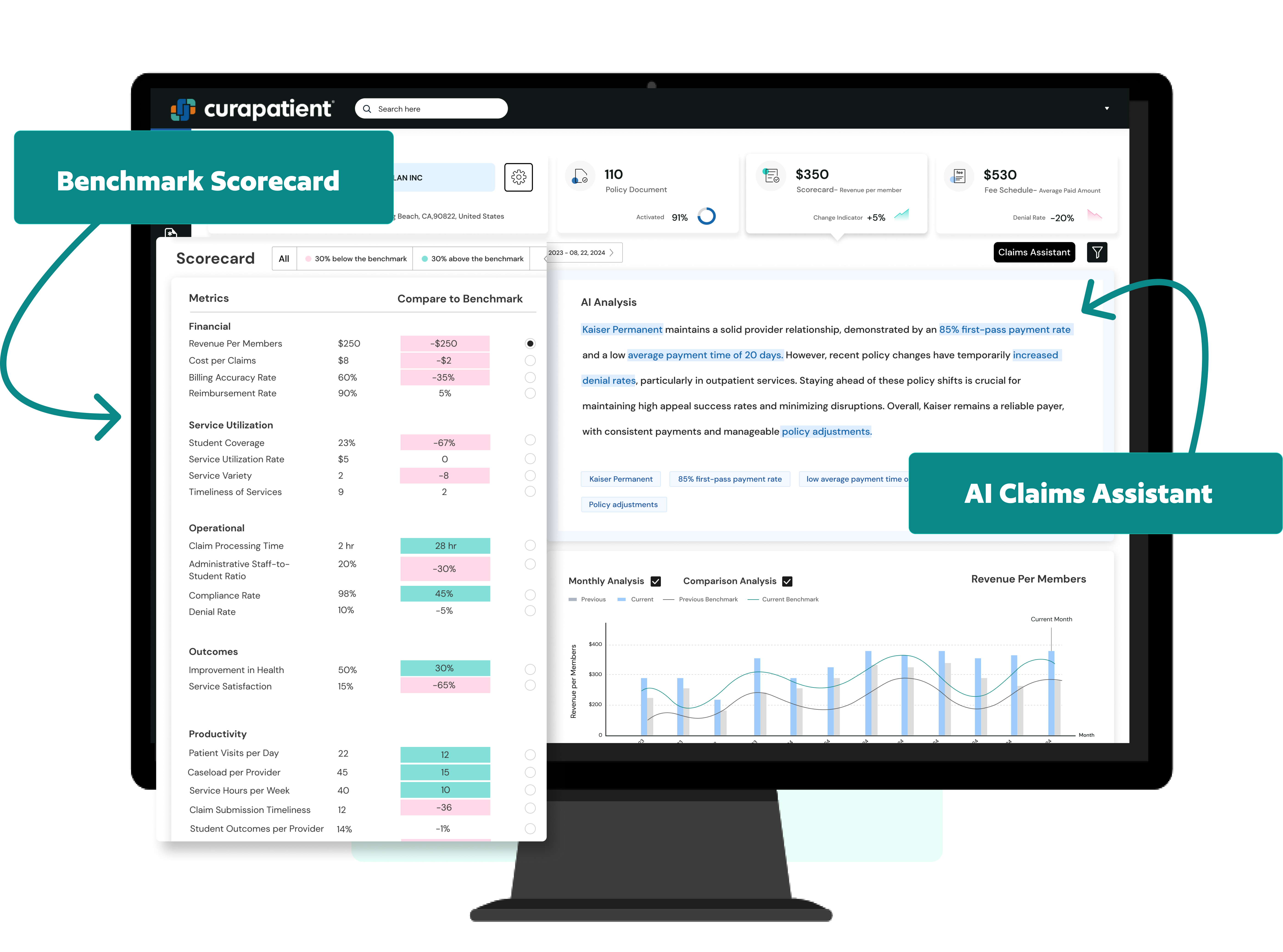
Optimize Provider Relationships
Review current accounts receivable and claims to challenge denials, recover underpayments, and identify retroactive claims for recovery.
Reinforced Learning Architecture
Gain valuable insights into payer patterns to ensure fair claim resolutions.
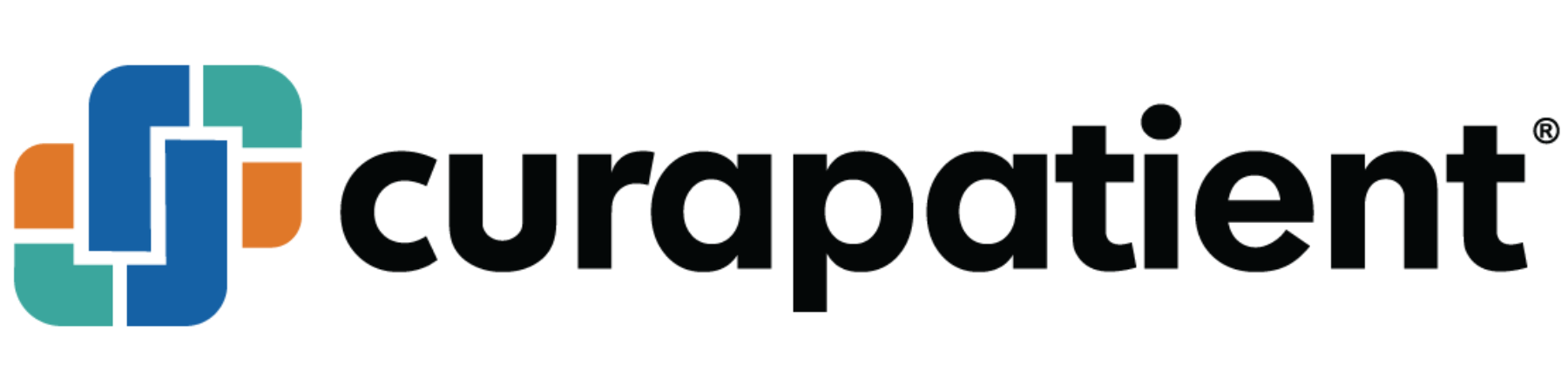
CuraClaims Features
Explanation of Benefits
Enhances our members’ experience by providing clear and comprehensible EOBs, keeping members well-informed and supported every step of the way. Our AI agent allows patients and users to be able to better understand their benefits and address requests from insurance companies.
Transparent Claims Valuation
Analyze each claim by considering contracts, procedures, local ordinances, and court rulings to ensure confidence in the outcomes. With a trained AI-assistant that understands:
• Physician-ready encounters, including summary information and relevant EMR data
• Benchmark metrics to eliminate hallucinations & assess effectiveness
• Staff training and education on key topics
Payer Behavior Insights
With an AI model trained on contracts, amendments, fee schedules, and payer behavior – our AI agent, specialized for every payer, can be seamlessly embedded into your operations.
Help Shape the Future of Healthcare
Request a Demo